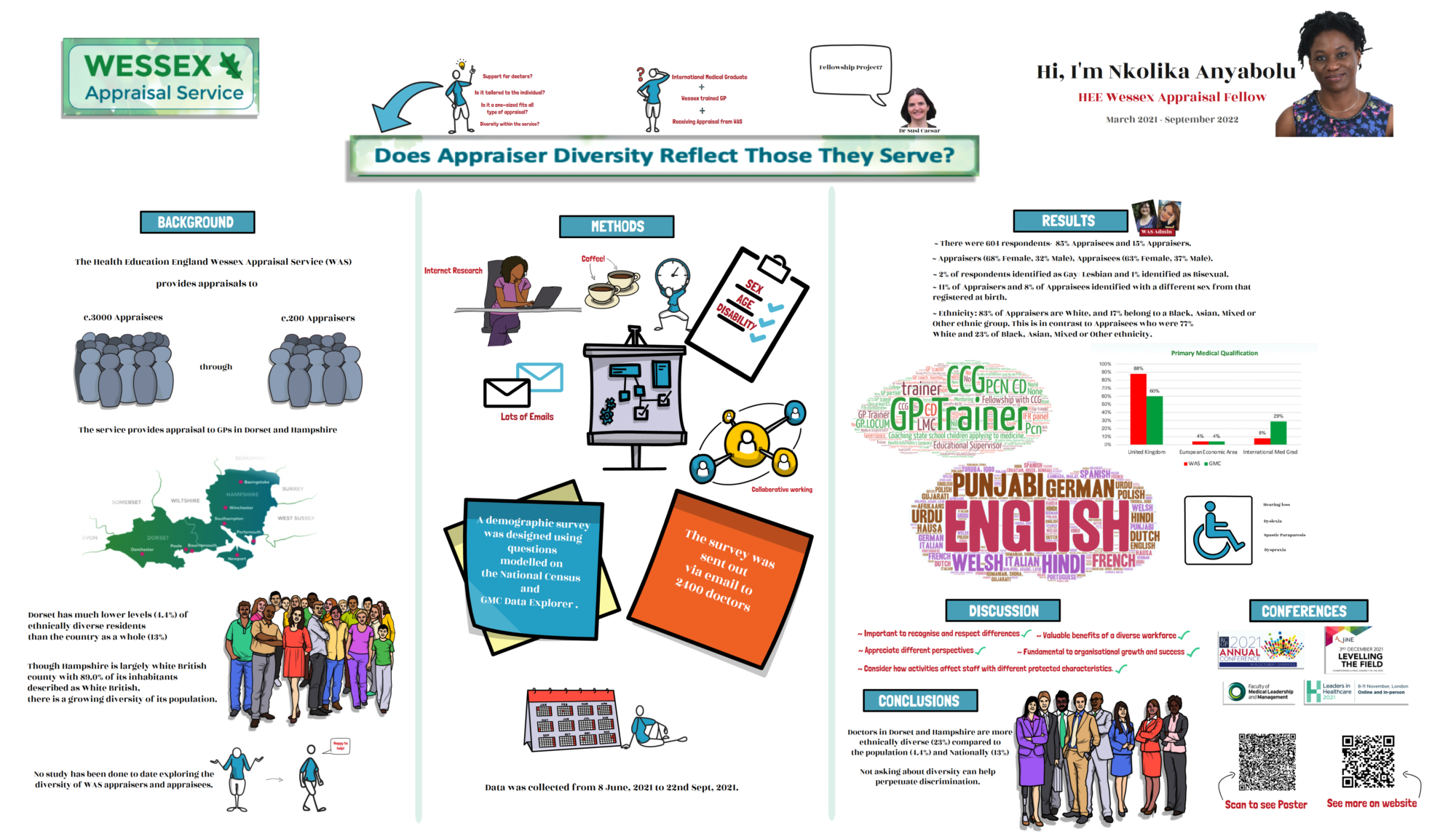
International Medical Graduates in Wessex Deanery
When I was appointed an International Medical Graduate (IMG) Fellow by the Wessex Deanery, I was particularly keen to find out more about the cultural barriers, which have a lot of impact on the performance and integration of IMGs in Wessex.
I knew they existed because as a Wessex trained GP I was well aware of the barriers I faced while I was going through the training programme.
I decided to research online to find out if there were similar problems elsewhere that have been published. I was amazed by how much work has been done in the area of issues IMGs face when working in the countries they have chosen to settle in.
International medical graduates (IMGs), by definition, move from the country in which they received their training to another country in which to train and/or settle down. IMGs historically have had remarkably diverse backgrounds, from cultures that are often radically different from the UK culture.
Cultural differences are a widely neglected topic both in equivalency exams that IMGs need to undertake before they are provisionally or fully licensed to practice or in empirical research with regard to IMGs [1–3].
These Cultural Issues affect IMGs’ learning and integration into the UK system [4] which in turn explains why IMGs have, on average, poorer outcomes in assessments and recruitment compared to UKGs1[5][6].
It is also notable that the most marked differential outcomes between UKGs and IMGs are in specialities in which patient-doctor communication is a key focus, such as GP and psychiatry.[7]
For IMGs to be successfully integrated into the UK system, conscious effort needs to be directed toward the facilitation of their acculturation into the UK society at large and the UK medical environment in particular. IMGs’ acculturation into the norms and standards of medicine as practised in the UK is crucial to their education as well as to the provision of quality patient care.
The time has come for the deanery to begin to systemically and effectively address the cultural challenges that IMGs face not only within the context of UK medicine but in the larger context of UK culture [9].
Specific programs and strategies need to be developed and put in place early to assist IMGs in understanding the cultural issues that may not even be apparent to them, which if left unaddressed will continue to impact their performance.
PROBLEM
IMGs represent an increasing proportion of doctors working in the UK. They come to the UK from diverse cultures around the world to work as speciality trainees, GPs, Physicians, SAS Doctors or Trust doctors. These doctors are and will continue to be a fundamental part of the UK health care delivery system.
They are more likely to fail postgraduate assessments and have poorer outcomes in recruitment compared to UKGs [5].
Differences in the average performance of groups with and without protected characteristics are called Differential Attainment. Though it is important; unfortunately the causes are still very poorly understood [4].
There are many factors that play a role in the performance of IMGs in the Wessex Deanery and the most important, and undoubtedly also the most complicated one is that relating to Cultural Issues. These Cultural Issues affect IMGs’ learning and integration into the UK system [4].
With the ongoing plans by the Deanery to recruit more IMGs through the Widening Access to Specialty Training (WAST) Scheme [10] and the Medical Training Initiative programme [11] [12], which are advertised as ideal for IMGs and doctors wanting to become a General Practitioner or Psychiatrist in England; there is a clear need to seek ways of addressing this differential attainment.
To find out more about the specific culture-related issues IMGs in Wessex may face, trainer and trainee perceptions were explored through interviews and the common issues highlighted were:
Lack of familiarity with shared decision-making
Poor understanding of the structure of the hierarchies in the NHS.
Difficulty with patient-centred care.
Issues around communication.
These findings are not unique to IMGs in Wessex as demonstrated by the results of numerous international research projects and systematic reviews which have been done in this area [8] [4][13].
RECOMMENDATIONS
The proposed recommendations have been split into 3 groups based on the level at which action needs to be taken and their amenability to change [4]
A. MACRO LEVEL (POLICY)
There needs to be a willingness on the part of policymakers; to instigate change and implement policies that would encourage an atmosphere of acceptance for IMGs.
B. MESO LEVEL (INSTITUTIONAL)
Deanery led demonstration of the appreciation of diversity which would lead to a healthier, culturally rich learning environment for all involved in education. This can be achieved via Cultural Retreats, International Meals, Adjusted advising systems as well as ongoing Faculty reflection on the treatment of IMGs [13].
Medical Educators need to take cultural differences into account when training IMGs. It is very important to know who these IMGs are as individuals, as representatives of their diverse cultures, take time to learn their names, find out more about their previous experiences and how best to help them. Understanding the specific challenges for IMGs is very important as every IMG is unique.
Time must be identified in orientation programs and in ongoing conference schedules to ensure that the process of acculturation receives the attention and priority it deserves.
There needs to be an increased awareness of these cultural issues and this can be done via Cultural-Sensitivity training for IMGs and non-IMGs. The already available Culture Workshops being run at the deanery need to be promoted and access to it improved.
In order to have a more patient-centred approach, it is important to have a very good grasp of the English language. Communication Skills Intensive courses which would help understand colloquial speech, body language, speech inflexions and the nuances of the language would go a long way to improving IMGs ability to communicate better.
Introduce initiatives that encourage cultural pride and respect e.g posters around trusts with people from different cultures promoting cultural diversity.
Mixed IMG and UK Graduate support groups across all specialities.
There needs to be a more culture-centred approach to teaching both IMGs and UK medical graduates. This can be achieved through changes in orientation [13 ].
Support strategies for IMGs should focus on building cultural and interpersonal competence and confidence [6]
C. MICRO LEVEL (ONE-TO-ONE INTERACTIONS WITH TRAINEES)
Small group workshops for IMGs facilitated by IMGs who has been through the system. This would serve as a safe place for IMGs to discuss the issues unique to them.
Mentoring system where IMGs would be mentored by another IMG who is able to share their experiences and also provide guidance.
Improved trainer-trainee relationship.
It is clear that the issue is not just a UK problem but indeed a global one. Sensitivities around race also act as a huge obstacle. Sadly despite all the work that has been done in this area and recommendations made, the problem still exists.
My brother, an IMG who has reached the zenith of his chosen subspecialty and a trainer for junior doctors; has had several IMGs as trainees. He has not only had to draw from his own experiences but also from those of the IMGs with whom he comes in contact.
He always tells me we think we had it tough until we hear the stories of others and then realize our journey was not so bad after all. He sums it all up very aptly:
The challenge is for the UK to recognise that IMGs are fully trained, committed, and highly motivated doctors who seek only the opportunity to give their best for patient care. While they may not have fluency in the English language, they may not be conversant with the cultural norms in the UK, and they may have little understanding of the systems at work in the NHS; it must be remembered that they have studied medicine, and have taken some form of the Hippocratic Oath, taking a vow of ethics, patient centred care, and confidentiality.
It is worth considering the challenges that a UK medical graduate would face if they emigrated to ply their trade in Saudi Arabia, or China, for example - this is akin to cultural and societal dislocation felt by recent emigrants to the UK, working in the NHS.
Are you an IMG? I would like to hear about your journey and experiences.
REFERENCES
Kalra G, Bhugra DK, Shah N. Identifying and addressing stresses in international medical graduates. Academic Psychiatry. 2012;36(4):323–329. doi: 10.1176/appi.ap.
11040085 [PubMed]Khan FA, Chikkatagaiah S, Shafiullah M, Nasiri M, Saraf A, Sehgal T, et al. International medical graduates (IMGs) in the UK- a systematic review of their acculturation and adaptation. Journal of International Migration and Integration. 2014; p. 1–17.
Terry D, Lê Q. Social capital among migrating doctors: the “Bridge” over troubled water. Journal of Health Organization and Management. 2014;28(3):315–326. doi: 10.1108/JHOM-09-2012-0178 [PubMed]
Fair Training Pathways for All: Understanding Experiences of Progression. Final Report. Prepared for the General Medical Council https://bit.ly/2EYWXVU
The State of Medical Education and Practice in the UK. General Medical Council. London; 2015
Patterson, Fiona & Alexander Tiffin, Paul & Lopes, Safiatu & Zibarras, Lara. (2018). Unpacking the Dark Variance of Differential Attainment in Exams for Overseas Graduates. Medical Education. 52. 10.1111/medu.13605.
Wakeford R, Denney M, Ludka-Stempien K, Dacre J, McManus IC. Cross-comparison of MRCGP & MRCP (UK) in a database linkage study of 2,284 candidates taking both examinations: assessment of the validity and differential performance by ethnicity. BMC Med Educ 2015;15 (1):1–12.
Michalski K, Farhan N, Motschall E, Vach W, Boeker M. Dealing with foreign cultural paradigms: A systematic review on intercultural challenges of international medical graduates. PLoS One. 2017;12(7):e0181330. Published 2017 Jul 17. doi:10.1371/ journal.pone.0181330
Gerald P. Whelan, MD. Coming to America: The Integration of International Medical Graduates into the American Medical Culture Acad Med. 2005; 81:176–178
Widening Access to Specialty Training (WAST) Recruitment https:// specialtytraining.hee.nhs.uk/wideningaccess
Medical Training Initiative http://www.aomrc.org.uk/medical-training-initiative/
Medical Training Initiative, NHS Employers https://bit.ly/2TfEJlU
Cole-Kelly K. Cultures engaging cultures: international medical graduates training in the United States. Fam Med. 1994 Nov-Dec;26(10):618-24. Review. PubMed PMID: 7859952.